In 2017, Massachusetts experienced 1977 opioid overdose deaths. While this figure is certainly high, it actually represents an 8 percent decrease in overdose deaths from 2016, indicating that Massachusetts has begun to make ground in combating the opioid crisis. This progress can likely be attributed to a number of policy initiatives that the state has undertaken over the past several years, many of which have tried to synthesize several competing hypotheses for the cause of the opioid crisis into omnibus legislation.
Combatting the Crisis with Policy
Governor Charlie Baker has made addressing the opioid crisis a top priority of his administration. In 2016, Baker signed into law “An Act relative to substance use, treatment, education and prevention,” a major piece of opioid legislation which focused on restricting opioid prescribing. Most notably, this law established a seven-day prescription limit for all first time opioid users and minors receiving prescriptions.
The law also created a Prescription Drug Monitoring Program (PDMP) in Massachusetts. PDMPs make it more difficult for people to receive prescription opioids from a physician by allowing physicians to view the prescribing history of a given patient. These policies are intended to limit “doctor shopping,” or the practice of visiting several doctors in order to receive a high quantity of prescription opioids. Furthermore, this past August, the Baker Administration strengthened restrictions on prescribing through the Step Act, which made PDMP participation mandatory for all physicians.
In addition to further prescribing limitations, the Step Act also focused on increasing access to treatment programs. This law both increased funding for treatment programs and requires all licensed maintenance facilities to treat patients with Medically-Assisted Treatments (MATs). MATs, most commonly the opioids methadone and buprenorphine, are drugs which can satisfy opioid dependence without producing the same euphoric effect as heroin. As such, these policies together attempt to address the opioid crisis on two fronts, namely by curbing overprescribing while also expanding access to substitution treatment.
The Countervailing Effects of the Restrictions
These laws appear to have succeeded thus far in bending the rising trend of opioid deaths in Massachusetts. Curiously, the recommendations pursued in these policies seem to toe the line between two competing hypotheses for the rise in opioid overdose deaths. The standard narrative for the opioid crisis posits that over-prescribing by doctors has led to more people becoming addicted to opioids, and eventually, more overdoses. Following this logic, if policy could decrease initial access to opioids, then fewer people would become addicted. Accordingly, both acts severely ramp up restrictions on prescribing through PDMP and regimen duration limits.
However, much of the academic literature suggests that restrictions such as PDMPs are ineffective in lowering total overdose deaths. Several studies have in fact found that there is no statistically reliable relationship between PDMPs and overdose deaths.
Worse, PDMPs may actually be associated with increased overdose deaths, particularly those attributed to heroin. One study published in Drug and Alcohol Dependence finds that with the adoption of a PDMP in New York state, “morbidity attributable to heroin overdose continued to rise.” PDMPs and other restrictions on prescribing make it more difficult for people to access opioids from legal channels. Thus, if they are cut off from receiving opioids from a physician, yet still have a demand for them, people will seek illicit opioids on the black market.
These drugs are far more dangerous than those acquired through legal means because of the inherent lack of information surrounding substances sold on the black market. In underground markets, consumers are unable to have complete information about the true contents of a substance, for “[g]overnment quality regulation does not exist for illegal commodities, and buyers cannot complain about quality without incriminating themselves.” Consumers are more likely to overdose because they unknowingly use drugs that are far purer than expected or laced with highly potent drugs such as fentanyl.
Since 2015, in fact, the majority of opioid overdoses came from illicit drugs such as heroin and fentanyl — not from prescription drugs. According to Dowell, the increase in fentanyl deaths between 2015 and 2016 “is enough to account for nearly all the increase in drug overdose deaths” in this period.” As more people are cut off from legal channels by restrictions, these more dangerous street drugs are all that they can access. Given the influence of illicit opioids on the total volume of deaths and potentially adverse effects of PDMPs, it seems implausible that restrictions on prescribing have been greatly responsible for Massachusetts’s recent success in lowering overdose deaths.
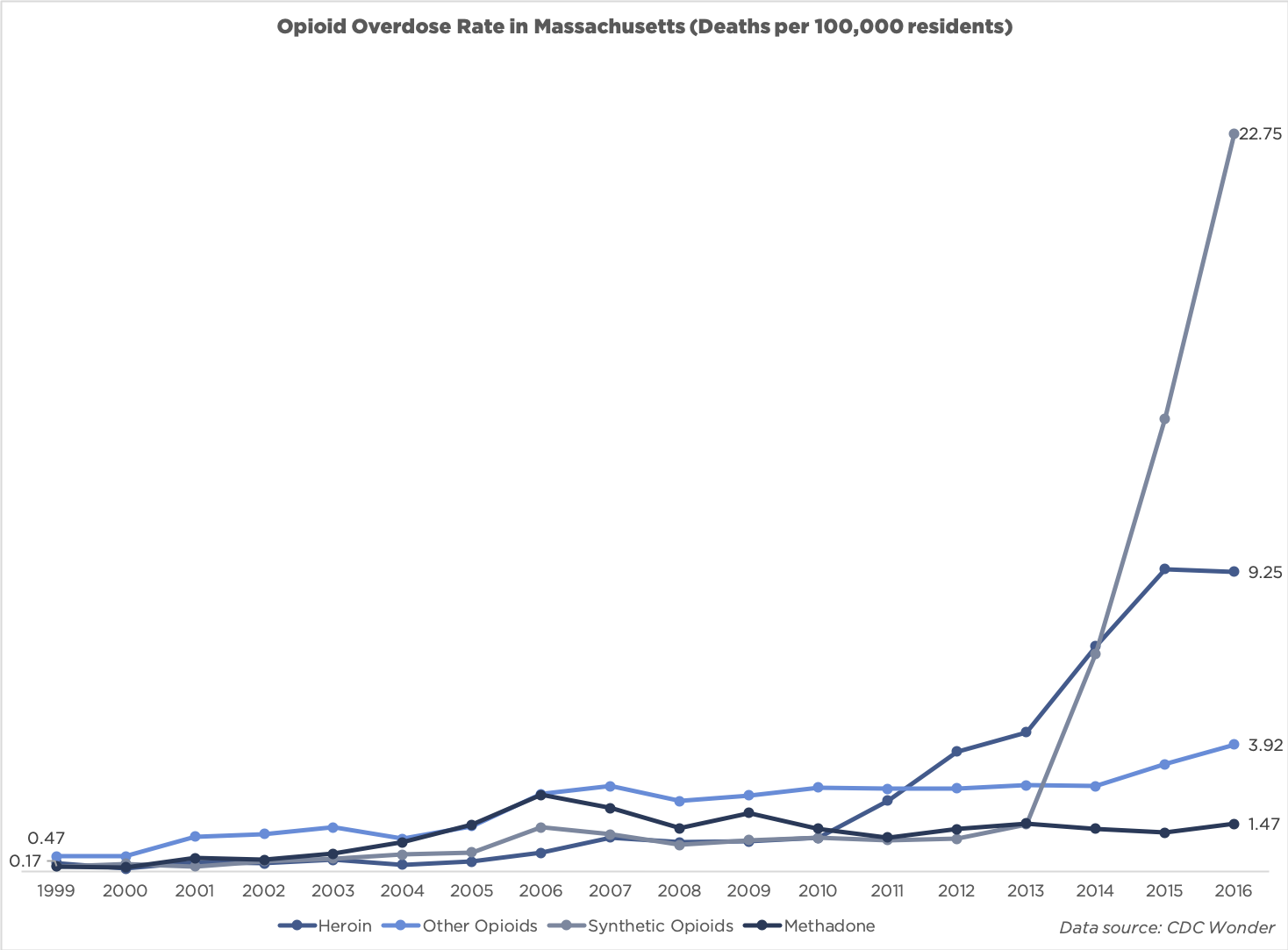
The overdose death rate per 100,000 in Massachusetts from 1999-2016 for various opioids.
Increased Safety Through Legal Access
In direct contrast to these restrictions on prescribing, recent legislation also expanded access to opioid treatments in Massachusetts. A competing narrative to the widely held belief that increased prescribing leads to increased deaths argues the opposite: increasing access to legal opioids would actually bring down the total number of overdoses. The Step Act does just this in expanding access to MATs, which can be administered in a safe, regulated setting.
Evidence suggests that increased access to these treatment opioids are associated with decreased overdose deaths. For example, a study conducted at the Boston Medical Center finds that “[t]reating opioid overdose survivors with buprenorphine or methadone was linked to a 40% to 60% drop in mortality 1 year later…” Instead of users being forced to seek out street opioids through illicit channels, increased access to opioids such as methadone allow for people to meet their demand for the drug legally and more safely. Because these treatment opioids are legally accessible, patients can know their exact contents and use under the supervision of a physician, greatly mitigating the risk of use.
Recent opioid legislation in Massachusetts thus seems to pick and choose policy recommendations from both narratives explaining the opioid crisis. While the state has expanded access to some opioids, it has restricted access to others, creating a sort of logically inconsistent mixed regime. Though it is unclear to determine exactly what share of the recent turnaround each policy is responsible for, the evidence suggests that while increased access to treatments may have helped reduce deaths, increased restrictions may have inadvertently stunted this progress.
If Massachusetts wants to continue breaking the trend in opioid deaths, it should focus on expanding access to legal channels for opioids rather than pursuing restrictive policies on prescribing, which may indeed be making matters worse. The progress that we have seen thus far in lowering opioid deaths in Massachusetts seems to be impeded by these laws which restrict prescribing. Well-meaning, yet misguided, intervention may be standing in the way of a more significant reduction in the overdose death rate.
Image Credit: Flickr/Marco Verch
